The year before someone’s 65th birthday is a great time for financial advisors to start talking about Medicare with clients. Starting Medicare may seem confusing and overwhelming for your clients, especially as they get inundated with insurance solicitations in the mail!
This article focuses on original Medicare, also called traditional Medicare, which is run by the federal government. The other option some clients may want to consider is Medicare Advantage, run by private insurers paid by the federal government. Advantage plans may work for some clients, particularly those who can’t afford the monthly cost of original Medicare. However, for those who can afford it and want broad access to doctors, original Medicare is usually the best choice.
If your client does want a Medicare Advantage plan, make sure they do their homework. Medicare Advantage plans often cover more services, but fewer medical providers accept those plans. After a few years on Medicare Advantage, it’s possible your client might decide they would rather be on original Medicare. Because original Medicare only covers 80% of medical bills, most likely that client will want a supplemental plan, too. But for some people, getting a supplemental plan at that point could be a problem because they’ll be required to go through medical underwriting. When you choose original Medicare during your first enrollment, you don’t have to go through underwriting for a supplemental policy.
Here are some questions that clients may ask you at various steps in the process about Medicare and the answers you will want to provide.
Step 1: Initial Enrollment
When should I enroll?
Although you’ll have a seven-month window to enroll in Medicare, in most cases you’ll want to enroll at the beginning of that period: three months before your 65th birthday. If you don’t already have one, create an account at the Social Security Administration, which runs Medicare. If you want to stay on employer-sponsored health insurance, you should check with Medicare to see if you’ll face penalties for signing up later.
I don’t want to sign up for my Social Security benefit. I want to wait to my full retirement age or later. Do I have to apply for Social Security when I enroll in Medicare?
NO. You do not need to sign up for your Social Security benefit. You can enroll in Medicare, which will be your insurance coverage only. There are three ways you can start the process with the Social Security Administration. SSA runs Medicare, so whether you want to start Social Security or not, you will need to work with SSA. You have three choices:
• Set an appointment with an agent in your local SSA office to see in person.
• Call and set a phone appointment with an agent in your local SSA office.
• Visit the Social Security website to enroll in Medicare benefits. (This is the easiest way.)
It is important that you start these steps three months before your effective date of Medicare. You want to give the government time to process your application. You will not be able to start your application any earlier than three months. This is an administration rule. There are 11,000 Medicare beneficiaries that turn 65 each day so you can imagine the flow of applications and processing timelines.
My birthday is on the 17th of the month so is that my effective date?
NO. Your effective date of coverage is the first day of your birthday month, if you enroll three months before. One exception: If you are born on the 1st of the month, your effective date would be the month before your birthday month. For example, if you are born April 1 your effective date would be March 1.
Step 2: Understanding the Cost
What does original Medicare include?
There are two parts that will take care of your medical needs.
• Part A (Hospital)
• Part B (Medical/Doctor)
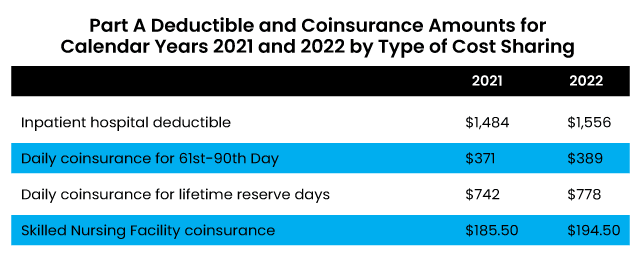
Medicare Part A will cover you when you are in the hospital. There are deductibles and co-insurance that you would need to pay the hospital. I have that included below. But if you sign up for a Medicare supplement policy or medi-gap policy (two names for the same policy), you won’t have to pay the Part A deductible and co-insurance.
There is no premium cost for Part A if you have worked a minimum of 10 years or 40 working quarters. This is your entitlement or “free benefit.”
Medicare Part B will cover everything outside of the hospital. That means doctor visits, outpatient procedures, MRIs, scans, blood draws and more. Part B covers 80% of those costs, leaving you with a decision on how to fill the gap for the additional 20%.
Medicare Part B does have a premium. The base premium for 2022 is $170.10 a month. This premium can be collected in a few different ways.
• If you aren’t on Social Security, you can choose to have quarterly bills sent to your house or a monthly bank draft from your checking account through an account you’ll need to set up on mymedicare.gov.
• When you are on Social Security, the premium is deducted monthly from your Social Security check.
Is there a deductible that needs to be satisfied for Part B?
Yes for 2022, the deductible amount is $233.
Can the government determine that I must pay more for my Medicare Part B premium?
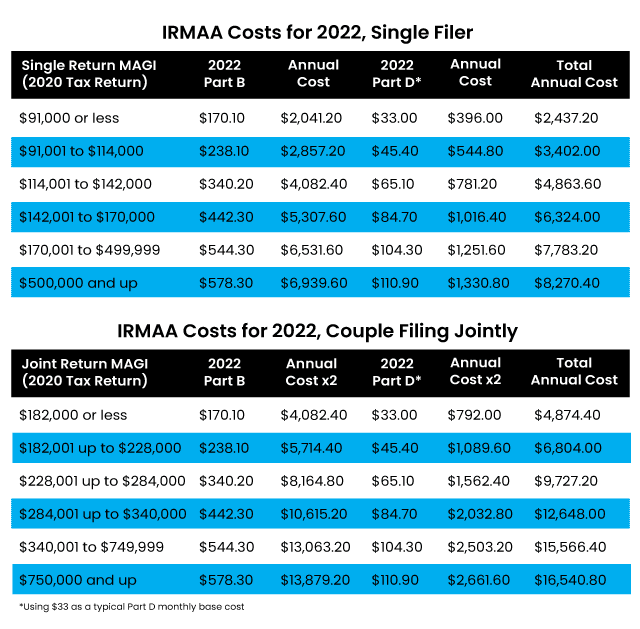
Yes. When you enroll in Medicare, the administration will connect with the IRS and look at your tax return for two years prior. If you were considered a higher earner, then you will have to pay an additional premium on top of your base Medicare Part B premium of $170.10. This is called Income Related Monthly Adjustment Amount or IRMAA. If they find that you will have to pay an additional premium, the administration will send you a letter explaining what you will have to pay. The IRMAA amounts are below for Part B, as well as for a drug plan (Part D).
If you disagree with the letter that you have received, you have the right to appeal. Many people do. The system is flawed. The administration is looking at your tax return two years prior. But now you are retired and no longer earning that income. To appeal, follow the directions in the letter that you receive. You can also appeal here.
Step 3: Choosing an Insurance Carrier
You will need to decide on a private Medicare Supplement carrier to close the gaps you have. Medicare does not pay for all your care. Depending on the state in which you live, there are many options of plans and carriers. Regardless of the plan options, the private insurance carriers all offer the same plan benefits but the prices are different.
Being that all the carriers offer the same coverage, I should just enroll in a plan the is cheapest, right?
WRONG. This is where you should lean on your trusted Medicare Supplement insurance broker and his/her knowledge of the market. Just because the rate is lowest does not mean the premium will stay low for the life of the plan that you are enrolled with that carrier.
There are some carriers that keep their rates low in the market because they are trying to gain quick market share. When that is obtained and the beneficiaries enrolled in that plan start using the coverage, there could be a spike in premiums.
So, if that happens I can switch plans?
The answer is it depends. Are you healthy? Depending on when you enrolled in your supplemental plan, you may have to go through medical underwriting to move to another carrier or plan. You should not have to take that chance. That is why it is important that you go with a carrier that has been in the market for a long time, is A-rated, and has a history of keeping its premium rates lower for longer.
Step 4: Choosing a Drug Plan
So, at this point in the process, your client has applied for Medicare Part A and Part B. You or they have identified what Medicare supplement plan they need to fill the gaps. The last step is to purchase a stand-alone drug plan. This is Part D of Medicare.
Will Medicare Part A and B and my supplement policy pay for my maintenance medication?
NO. You will have to enroll in a stand-alone drug program. This can be accomplished on your own or with broker assistance at Medicare.gov.
Looking up your drugs will give a good idea of what insurance carrier will be best for you for the year you enroll.
You should always review your maintenance medications during the annual election period (AEP). The time to do this is October 15 to December 7 every year.
I am not on any medications currently. I do not want to enroll in a drug plan. Can I skip it?
Not a good idea. Once your enrollment period closes you will not be able to obtain a prescription plan until the following year. Not only that, Medicare will penalize you with a late enrollment penalty for not enrolling into your prescription plan when you were first eligible for Medicare. That late enrollment penalty gets charged monthly for the rest of your time on Medicare! This could be a very costly mistake.
Step 5: Last Steps
By now, your client has enrolled in Medicare Part A and Part B. They have obtained a Medicare Supplement policy, and based upon their prescription needs, they have enrolled in a drug plan.
Tell your client to review all documents when they arrive in the mail, including: their Medicare ID card, to make sure it has the correct effective date; the Medicare supplement plan, to make sure it’s the plan they chose; and the drug plan, to ensure the enrollment date is correct.
When clients go to use Medicare, they should ask their doctor one question: Do you take Medicare? Most doctors will answer yes. If they do, they will automatically take the Medicare supplement policy.
How do I know if my doctor will take my supplement? Are they in my network?
Original Medicare is your primary insurance now. The Medicare supplement is your secondary. You no longer have any networks, co-pays, max out of pocket costs, pre-approvals, or prior authorizations. You have left managed care behind! Remember when you had to look up in a directory to see if your doctor participated? That is a frustration of the past. You are free to see any doctor you want! The secondary coverage, even though it is a private carrier, cannot dictate what it will pay for. If Medicare deems the procedure medically necessary, Medicare will pay and then the supplement will pay. This process is called auto adjudication. You, the consumer, are not involved in this process and that is a good thing!
Many doctors might not be contracted with the supplemental carrier. They are contracted with Medicare. So, when you see the doctor and they file a claim on your behalf to get paid, Medicare will pay its portion, then ask the supplemental carrier for the rest. The private carrier will pay Medicare and then those funds will be paid to the doctor or hospital.
Congratulate your clients! They have fantastic benefits, and they earned them!
Toby Stark, a licensed health, property and casualty agent, is founder of Stark Associates Insurance Agency in Tinton Falls, N.J. The majority of the firm’s clients are small to medium businesses that are looking for flexibility as needs and budgets change.







